DES is a synthetic oestrogen, prescribed to many pregnant women in the mistaken belief that it prevented miscarriage. The drug was used from the early 1940s to the early 1970s (and beyond). It is the story of the continued use of a drug despite evidence of its ineffectiveness and danger. It is the story of a time-bomb. The cancer and fertility problems in sons and daughters of those women who were prescribed DES are still unfolding. It is the story of the failure of the medical profession, health authorities and drug companies to face up to the problem and take action. The story is not only of past failure - crucial measures needed to deal with the time-bomb effects are still being ignored.
By Marian Vickers
(1985)
Beginnings
The promotion of DES as a treatment to prevent miscarriage and pregnancy complications came first from the prestigious Harvard Medical School in the early 1940s. Head of the Gynaecology Department at Harvard (1942-1967), Dr George van Sichlen Smith, and his wife Dr Olive Watkins Smith, began theorising about the new drug's use in maintaining high-risk pregnancies. The maternity hospital associated with Harvard was used by the Smiths to test their theories on pregnant women. Putting it bluntly, they were wrong. Their theory was wrong, their methodology shoddy and their analysis and interpretation of results subjective and suspect. The drug should never have been allowed on the market for use in pregnancy. Right from the start questions were asked about the effectiveness of DES. At the Annual Conference of the American Gynaecology Society in 1949, a doctor challenged the Smiths' theories, and pointed out that: "(In the pregnant rabbit) the administration of oestrogen is very deleterious to the foetus. In early pregnancy, oestrogen will prevent implantation or produce abortion; and during later stages it will lead to death of the foetus."
The Smiths' methodology for their studies was criticised. The controversy itself led to many "experiments" being conducted on unsuspecting women attending hospital ante-natal clinics (including here in Australia), in attempts to verify or disprove the Smiths' rather exuberant claims for the new "wonder drug".
In 1953 a large, well-designed, prospective, double-blind study (involving 2,000 unsuspecting "subjects"!) showed that DES was no more effective in preventing miscarriage than the placebo given to the control group in the study. Despite the mounting evidence, the use of DES as a therapy for pregnancy maintenance continued. The Smiths strongly defended their research and continued to advocate the use of DES. As they were associated with Harvard Medical School, their claims were influential. And the drug companies certainly jumped on the bandwagon - taking out full-page advertisements in the medical journals, citing the favourable research. They were not about to mention the studies which called into question the drug's efficacy.
Spread to Australia
In Australia, many obstetricians/gynaecologists were impressed with the claims made by the Smiths; and prescribed the “Smith regimen” of large and increasing amounts of the drug throughout the entire pregnancy, starting when pregnancy was first confirmed. Other obstetricians/gynaecologists appear to have been more hesitant. Some seemed to have taken a punt both ways: Not wholly convinced of the claims but, as “it did not harm”, they prescribed smaller amounts of the drug – presumably so the high-risk patient would be reassured by thinking something was being done to maintain her pregnancy. With DES mothers sharing stories we have been able to track the prescribing practices of a number of doctors. From tentative beginnings in the early 1950s (one table per day), by the mid-1950s the “Smith regimen” was being prescribed - “I had it by the bucketful”, to quote one mother. The obstetricians/gynaecologists who advocated the use of DES spread the “good news” to their GP colleagues. Unfortunately when DES fell from favour among the specialists and was replaced by other hormonal therapy (notably progesterone), they often failed to mention it to the GPs who kept on prescribing DES. DES was also used for purposes other than maintaining pregnancies. Ironically, it was used as a contraceptive "morning-after" pill, that is, to supposedly induce spontaneous abortion. If it did not work, and the pregnancy continued, then the foetus was exposed to DES. It was used to suppress lactation and dry up breast milk. Teenage girls were prescribed DES as a treatment for acne. Hormonal pregnancy testing was popular during the 1960s and 1970s. All these uses exposed further people to DES.
The Time Bomb
DES has been likened to a time-bomb. At the time it was first prescribed, it was assumed safe by prescribing doctors. But its effects on the children of women prescribed DES would reveal, in time, how wrong this was. In the late 1960s, over 25 years after DES was first prescribed, eight young women (11-22 years old) were admitted to Massachusetts General Hospital with an aggressive form of cancer of the vagina and cervix known as clear cell cancer. Until this time, this was an exceptionally rare cancer occurring in women after menopause. In the entire world's medical literature there were only three cases reported of this cancer developing in young women. Suddenly there were eight in the Boston area.
Looking for the cause for the sudden emergence of this cancer in young women factors such as douches, tampons, the contraceptive pill, sexual promiscuity, maternal smoking and pre-natal X-rays were eliminated. Finally, one of the mothers made an intuitive guess that the cause might be the DES she was prescribed during pregnancy. It was then confirmed that seven of the eight mothers had taken DES during pregnancy. DES was thus proven to be a trans-placental carcinogen. The results were published in 1971 by the New England Journal of Medicine. A registry was established to record the incidence of the rare cancer. Within two years, 170 cases were registered. Currently there are over 500 listed. Since it is not mandatory to report cases to the registry, this is obviously not the complete incidence and the true tally will probably never be known.
Since these initial ominous revelations, more effects of DES have emerged and been reported in medical journals with varying degree of detailed study. Space permits only a few to be mentioned here:
- Many DES daughters have benign tissue and structural changes to the vagina and cervix relating to their DES exposure.
- Abnormalities of the uterus and fallopian tubes have been found in DES daughters. The most common and characteristic change is a T-shaped uterus with a small uterine cavity. These abnormalities are suspected as possible causative factors in the higher incidence of pregnancy difficulties experienced by many DES daughters.
- DES daughters have a high incidence of pregnancy difficulties. When compared to a non-exposed control group, DES daughters experienced a 3-5 times higher rate of ectopic pregnancy; at least twice the rate of miscarriage in the first and second trimesters; and at least three times the rate of premature labour, premature birth and stillbirth. It appears that as many as 50% of DES daughters will experience these reproductive complications. Researchers generally agree that about 80% of DES daughters who conceive will, if they "keep trying", eventually have at least one living child. That is, of those DES daughters able to conceive, approximately 1 in 5 will never have a "viable outcome" despite numerous "tries". This statistic hides a great deal of human pain and sadness, as any DES daughter at present experiencing "non viable outcomes" will tell you.
- Recent research findings have revealed that DES daughters have between a two- and four- fold increased incidence of dysplasia and squamous cell cervical cancer.
- Approximately a third of DES sons have structural abnormalities of the genital tract, including higher rates of undescended testes (a known risk factor for testicular cancer).
- A study last year, using matched control groups, indicated that DES mothers, themselves have a moderate (40-50%) statistically significant increased risk of breast cancer in later life, i.e. 20-25 years after taking DES.
The alarming thing is that we don't know what further health problems may arise in DES exposed people as they get older. The Medical Journal of Australia (MJA), last year, reported the following comments by Dr Michael Coppleson, Head of the Gynaecological Unit, King George V Memorial Hospital, Sydney: "What is the likely fate of the (DES) exposed progeny? It is possible that their tumour incidence may rise, and that the types of tumour may alter as the population gets older. In women, it is clear that the breast must still be regarded as predisposed to neoplasia, as well as other mullerian derived tissues, including the endometrium. In men, the prostate may be the organ on prime risk. Many more years of careful follow-up of all progeny - both male and female - exposed as foetuses to DES will be required before a precise assessment of all detrimental consequences is possible. This survey should include a search for tumours in the mothers and their DES exposed sons and daughters, as well as for adverse effects on fertility and pregnancy."
Response of the Australian Health Care System
The Australian response since the effects of the drug have been known gives further cause for major concern about the Australian health system's ability (or inability) to respond to a major public health issue.
Let's go back to 1971: DES constituted a potential medical crisis in terms of public health. There was sudden emergence of a previously rare cancer. This cancer was very aggressive, essentially symptomless, and required special screening tests (a Pap smear test not being adequate). The victims were young females and the treatment was drastic, including radical hysterectomy and vaginectomy. At this stage (early 1970s), the cancer had a high mortality rate, and its potential incidence among DES daughters was unknown - 3 cases in the world, then 170 within two years. In addition, this cancer was caused by a medical treatment which had been in use for many years.
A rational approach would include a head count. How many women have been prescribed this drug during pregnancy? How do we alert them to the risk? That is, there was an obvious and urgent need to identify and alert the population at risk and provide appropriate medical care. Now, what happened in Australia? From the consumer's viewpoint, and for all practical purposes, nothing! Tucked away in the MJA of September 1972 is a statement by the Drug Evaluation Committee, which includes: "As far as can be ascertained, stilboestrol has not been used to any extent in this country for the management of threatened abortion…" Based on what? There has never been any attempt to estimate the extent of DES exposure in Australia. The statement then goes on to conclude: "It is reasonable to conclude that stilboestrol should not be given in pregnancy." Rather mild, don't you think? As a 1981 editorial in the MJA points out: "In Australia... no adequate records of children exposed to DES exists. There has been no organised publicity, or any systematic education or follow-up campaign, and there is understandable apprehension amongst the Australians who suspect that they may be at risk."
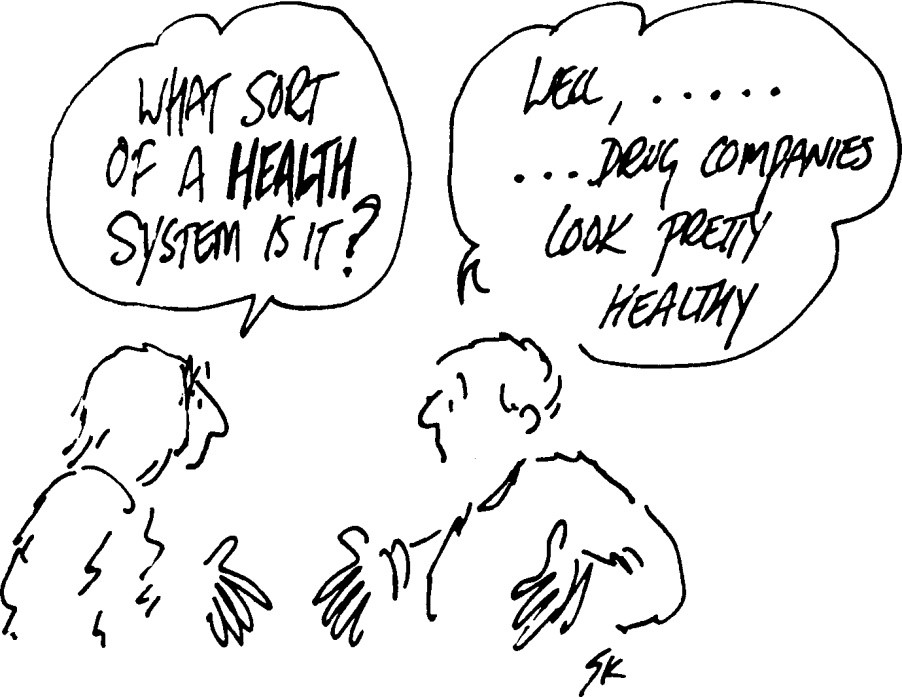
Of great concern to the whole community should be the fact that, both here and in the US, it was only after consumer groups organised that any serious attempt was made to alert the population at risk and provide accurate, sensible information on their health risks and the appropriate health care needed. That is, this was done by consumers, for consumers. The response of the Australian health authorities has been to continually minimise, deride and trivialise DES-exposure, both at the personal level and as a public health issue. Why? DES is a medical treatment and DES related problems are the direct result of a medically prescribed drug. The Ministers of Health, the health authorities, and for that matter the medical profession itself, take advice on the DES question from a group of doctors who, in a sense, helped create the problem and who have every interest in seeing that the issue is minimised.
Is There More?
The number of Australian women prescribed DES and related drugs during pregnancy is still unknown. We know that DES was used throughout Australia, in every State, in capital cities and in country areas. However there has never been any concerted effort or co-ordinated official attempt to identify and alert the Australian DES population. Major ongoing research is not being done. This highlights the fact that much medical research is funded by the drug industry, and no drug company is going to fund research into the effects of DES. Financial support is needed for consistent, long-term follow-up of DES mother, daughters and sons. Research is needed that considers a broad range of all possible DES effects as the DES population grows older. If additional health problems emerge, they can be detected early, or reassurance can be gained if no new problems appear. DES is only one type of oestrogenic exposure. It is an unfortunate but nevertheless real human experiment that should be faced, not only for the welfare of the exposed population but also for the knowledge it may reveal which could be relevant to other drugs. There may be other drugs that have or will have this time-bomb effect and public health strategies should be worked out now, based on the DES experience.
Published in Health Action, journal of the Health Issues Centre, November/December 1985. It provides a comprehensive overview and summary of what was know about DES at that time.